Applied Policy’s CEO Jim Scott and Vice President of Healthcare Services Carl Mallory were among the approximately 1,000 attendees at the American Hospital Association’s (AHA’s) Annual Membership Meeting, held April 14-16 in Washington, D.C.
The event, which brought together hospital presidents, CEOs, administrators, and senior executives, afforded an opportunity for Applied Policy to speak with healthcare leaders from across the country and to further its appreciation of AHA’s advocacy and policy priorities.
Key Issues
The topic of prior authorizations received significant attention, both in formal sessions and informal conversations among participants. A growing concern for providers, hospitals, and patients alike, prior authorization requirements contribute to administrative burdens and can result in critical delays in treatment or the denial of definitive care.
AHA had previously lauded the Centers for Medicare & Medicaid Services (CMS) for its final rule regarding transparency in the prior authorization process in Medicare Advantage and CMS Administrator, Chiquita Brooks-LaSure received a warm response for her remarks on the subject.
In a separate session, Kurt Barwis, President and CEO of Bristol Health and an AHA board member, said that he believes CMS has done “a great job of going after prior auths.” However, he agreed with other panel members that much work remains to be done.
Workforce issues were another key focus of the event, as American hospitals face what the AHA has characterized as “a national staffing emergency.” Sen. Dick Durbin (D-Ill.) discussed the Healthcare Workforce Resilience Act, which would expedite the authorization of visas for certain healthcare workers, and the Restoring America’s Health Care Workforce and Readiness Act, which would increase enhanced funding for the National Health Services Corps (NHSC) through FY2026. Both bills have bipartisan support.
The conversation about workforce issues extended to discussions of worker safety. Stacey Hughes, AHA’s executive vice president for government relations and public policy, emphasized the need for co-sponsors for the Safety from Violence for Healthcare Employees (SAVE) Act. The bill, which was introduced by Rep. Larry Bucshon (R-Ind.-08) and Rep. Madeleine Dean (D-Pa.-04) last year, would make the assault or intimidation of hospital personnel a separate category of criminal offense, extending hospital workers federal law enforcement protections similar to those currently afforded to commercial flight crews.
While sessions on cybersecurity had been scheduled before the Change Healthcare cyberattack, the historic security breach highlighted their importance. Attendees were eager to learn what steps the federal government was taking to support hospitals in the wake of the breach and to prevent future attacks. They also wanted to learn more about what steps they could take to protect their own organizations and patients.
In conversation with John Riggi, AHA’s national advisor for cybersecurity and risk, Anne Neuberger, deputy assistant to the president and deputy national security advisor for cyber and emerging technology on the National Security Council, said that cyberattacks against the healthcare sector in 2023 increased 120% over 2022. Observing that U.S. entities paid $1.3 billion in ransom for cyberattacks in 2023, Neuberger cautioned, “Every ransom payment feeds the beast and brings on the next attack because it further incentivizes the attackers.” She referred attendees to the voluntary consensus-based cybersecurity practices released by the Department of Health and Human Services (HHS) through the Administration for Strategic Preparedness and Response (ASPR) in January.
Speaking specifically of the Change Healthcare attack, HHS Deputy Secretary Andrea Palm observed, “We’ve been in a live fire exercise recently and are learning lessons that inform the ways we will move forward.” In a comment that echoed Applied Policy’s story on cybersecurity earlier this year, Sen. Ron Wyden (D-Ore.) observed that the “healthcare sector is a prime target for criminals and foreign adversaries like China and Russia.”
Although the Rural Washington Update session addressed rural healthcare directly, the difficulties faced by America’s rural hospitals echoed throughout most sessions. In the Federal Forum Plenary, Rep. Morgan Griffith (R-Va.) spoke of the importance of telehealth for rural healthcare, and Sen. Wyden referenced the plight of rural hospitals. Separately, Deputy Administrator Palm acknowledged that rural hospitals were uniquely challenged in terms of cybersecurity. One of the more moving recognitions of the importance of rural hospitals was the awarding of the 2024 Board of Trustees Award to Christina Campos, the CEO of Guadalupe County Hospital, a 10-bed general acute care hospital in Santa Rosa, New Mexico.
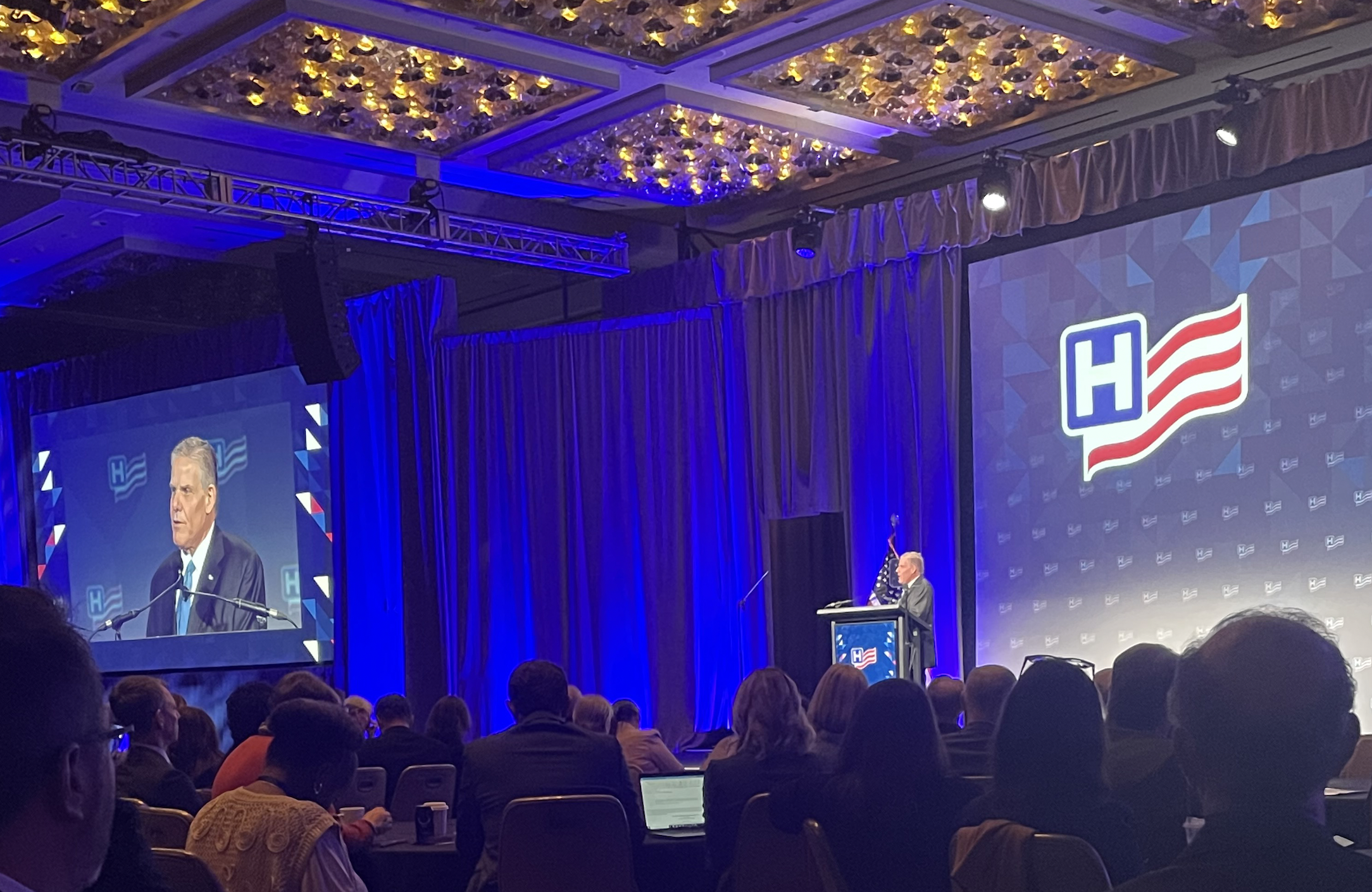
Given its importance and the fact that the meeting was hosted in the nation’s capital, it was unsurprising that many members of Congress, the Administration, and the media were present in either formal or informal capacities. White House Domestic Policy Council Director Neera Tanden spoke of the Biden Administration’s healthcare priorities. Former Speaker of the House Kevin McCarthy joined the Federal Forum panel as a private citizen able to share insights from his time in Congress. The founders of Punchbowl News shared insider perspectives on politics. However, the most popular participants may have been the therapy dogs holding court at the Pup Station.
Ultimately, the commitment of attendees may have been best expressed by Brian Gragnolate, President and CEO of Atlantic Health System. In accepting the 2024 Distinguished Service Award, he observed that “healthcare truly is a team sport where human beings care for human beings.”
Below left: Applied Policy President and CEO Jim Scott with CMS Administrator Chiquita Brooks-LaSure.
Below right: Applied Policy Vice President for Healthcare Services Carl Mallory speaks with AHA President and CEO Rick Pollack.



