
On July 30, 2019, the Centers for Medicare & Medicaid Services (CMS) released their Skilled Nursing Facility (SNF) Final Rule for Fiscal Year 2020. Overall, CMS estimates that total payment to SNFs will increase by $851 million in FY 2020.
Major finalized provisions within the rule include expansion of the window to complete an initial patient assessment, loosening the definition of group therapy, and finalizing several provisions within the SNF Quality Reporting Program (QRP). CMS chose not to finalize their proposed requirement for all-payers to report on SNF quality measures. This final rule becomes effective October 1, 2019.
SNFs to See Payment Increase in FY 2020
Initially adopted in the FY 2019 final SNF payment rule, CMS is continuing to implement a new case-mix classification system for classifying SNF patients, called the Patient Driven Payment Model (PDPM). The PDPM classifies patients into groups based on patient-characteristics instead of using volume of therapy services as the basis for payment classification. The PDPM is being implemented in a budget neutral manner.
CMS finalized the following unadjusted federal rates based on the PDPM:
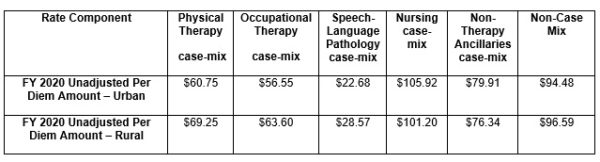
Overall, CMS is estimating that total payment to SNFs will increase by $851 million in FY 2020. The SNF market basket growth rate is 2.8 percent for FY 2020; this rate is then reduced by the multifactor productivity adjustment of 0.4 percent for FY 2020. SNFs that fail to report the required quality data will have a 2 percent reduction applied to their payments.
Definition of Group Therapy Loosened in SNF Setting
CMS is finalizing their proposal to change the definition of group therapy from exactly four patients to between two and six patients; these patients must be performing the same or similar activities. This new definition of group therapy will align with other Agency initiatives such as the Meaningful Measures Initiative and provisions included within the IMPACT Act. Therapists must document the need for group therapy with each patient, as the Agency feels that individual therapy is the most effective way to deliver Occupational Therapy, Physical Therapy, or Speech-Language Pathology services. The majority of commenters on the SNF proposed rule supported updating this definition of group therapy.
CMS Finalizes Sub-Regulatory Process to Update ICD‑10 Codes Under PDPM
Under the establishment of PDPM, ICD-10 codes are used to assign patients into case-mix groups instead of by the traditional volume of services. As ICD-10 codes have the opportunity to be updated twice annually, CMS finalized their proposal to update non-substantive ICD-10 codes via the PDPM website, stating that publishing updates on the website will allow clinicians to have the most up to date information.
Comments on this provision were generally supportive. CMS will use this new sub-regulatory pathway for non-substantive changes only; the current rulemaking process will still apply to substantive changes to the ICD-10 code set. CMS further defines a substantive change as one that would be of any change that goes beyond the intention of consistency changes.
Eight-day window for Completion of Initial Patient Assessment finalized for FY 2020
CMS currently requires a functional assessment of patients no later than five days after admission to a SNF. However, CMS has always recognized a three-day grace period for completion of an initial patient assessment, meaning that CMS would accept an initial patient assessment if completed within eight days. CMS is finalizing their proposal to formally expand this assessment requirement from five days to eight days. Further, CMS is changing the assessment title from the “five-day-assessment” to the “initial patient assessment” to reflect this change.
CMS Adopts Two New Quality Measures for SNfs But Decides Not to Finalize All-Payer SNF Quality Reporting
In the FY 2020 proposed SNF rule, CMS proposed to expand quality reporting to all SNF residents, regardless of payer, to ensure that Medicare residents received equivalent treatment to non-Medicare patients. However, in response to comments regarding the burden of this data collection, CMS has decided not to finalize this proposal, but rather to make additional changes and issue a new proposal in future rulemaking.
CMS is finalizing their proposal to adopt two new measures into the SNF Quality Reporting Program (QRP) in line with the agency’s Meaningful Measures initiative:
- Transfer of Health Information to the Provider-Post Acute Care (PAC)
- Transfer of Health Information to the Patient-Post Acute Care (PAC)
The agency is also finalizing their proposals to publicly display the Drug Regimen Review Conducted with Follow-Up for Identified Issues- Post Acute Care (PAC) and to exclude baseline nursing home residents from the Discharge to Community measure.
No Major Changes to SNF Value-Based Purchasing Program in FY 2020
No major changes were proposed for the SNF Value-based Purchasing Program (SNF VBP). There will be no changes made to the SNF VBP scoring or payment policies for FY 2020. The performance period for the FY 2022 SNF VBP will be FY 2020 and the baseline period will be FY 2018. CMS did finalize the proposal to change
CMS is finalizing their proposal to include the following information for SNFs on the Nursing Home Compare Website:
- SNFs with fewer than 25 eligible stays during the baseline period will not have baseline risk-standardized readmission rate (RSRR) or improvement scores displayed but performance period RSRR, achievement score, and total performance will be displayed if there are sufficient data;
- SNFs with fewer than 25 eligible stays and that receive an assigned SNF performance score will have the assigned performance score reported but the performance period RSRR, achievement score, and improvement score will not be displayed; and
- SNFs with zero eligible cases during the performance period will not have any display information.
Applied Policy in the News
x
Meet the Team
x
Philanthropy
x


