
On July 31, 2019, the Centers for Medicare and Medicaid Services (CMS) released the final FY 2020 hospice payment rule. The proposal finalizes an overall payment increase for hospices as well as rebased rates for three levels of care.
Provisions of this final rule take effect on October 1, 2019.
Per Diem rates rebased for chc, irc, and gip levels of care; payments to hospices expected to increase in fy 2020
Overall, CMS is estimating a $520 million in increased payments to hospices for FY 2020. The payment update for hospices will be 2.6 percent in FY 2020. Hospices that do not submit the required quality data will be subject to a reduction of two percentage points, meaning a 0.6 percent payment update.
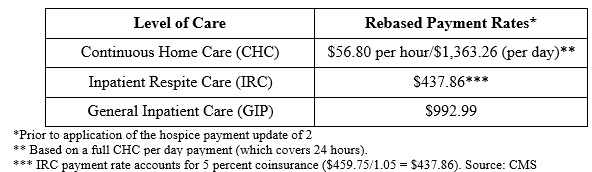
CMS is finalizing their proposals to rebase the FY 2020 per diem rates for continuous home care (CHC), inpatient respite care (IRC), and general inpatient care (GIP) levels of care by setting these amounts equal to the FY 2019 estimated average costs per day. This is done before application of the hospice payment update percentage, which is 2.6 percent for FY 2020. The rebased amounts for these levels of care are:
Updates to hospice payment must be made in a budget neutral manner. To maintain budget neutrality after rebasing the CHC, IRC, and GIP levels of care, CMS is finalizing their proposal to reduce the routine home care (RHC) payment amounts in FY 2020 to . A 2.72 percent reduction will be applied to RHC payment rates for FY 2020.
CMS if finalizing a hospice cap amount of $29,964.78 for FY 2020. This is equal to the FY 2020 cap amount updated by the 2.6 percent FY 2020 hospice payment update percentage, as required by statute. CMS is also finalizing its proposal to remove the one-year lag in data by using the current year wage data to establish the hospice wage index.
CMS finalizes hospice election addendum proposal, cites increased transparency as some commenters express concerns over administrative burden
CMS is finalizing a requirement for hospices to include an addendum to patients, titled “Patient Notification of Hospice Non-Covered Items, Services, and Drugs.” This new signed addendum will also serve as a new condition for payment.
Currently, hospices are required to provide a statement to patients after an initial evaluation that outlines all anticipated services under hospice care. However, this new requirement expands upon this practice, requiring hospices to also provide:
- Information about the holistic, comprehensive nature of the Medicare hospice benefit;
- A statement that, while rare, there might be necessary items or services not covered by the hospice;
- Information about beneficiary cost-sharing for hospice services; and
- Notification of the right to request an election statement addendum of a written list and rationale for the conditions, items, drugs, or services the hospice determines are unrelated to the terminal illness and that advocacy is available if the beneficiary or representative disagrees.
Comments on this new addendum provision were mixed; several applauded CMS’ steps towards transparency, while other stakeholders cited increased administrative burden. This effort is part of the agency’s larger initiative to increase transparency for patients, enabling increased patient participation in the choice of providers and services they use.
automatic volume exemption for cahps survey data and public posting of government data to hospice care website finalized
The Hospice Quality Reporting Program (HQRP) uses the CAHPS Hospice Survey to collect data on patient and caregiver experience. CMS previously finalized a volume-based exemption through FY 2021. In this rule, CMS is finalizing an automatic exemption to hospices that are an active agency and have served less than a total of 50 unique survey-eligible decedents/caregivers in the reference year. This exemption will begin in FY 2022 and the automatic exemption would be good for one year. CMS is also finalizing their proposal to extend existing participation requirements for the Hospice Quality Report System (HQRP) to FY 2023 and all future years.
Data submission will be migrating to a new internet Quality Improvement and Evaluation System (iQIES) as soon as FY 2020 for hospices. Beginning October 1, 2019, CMS will notify the public about the migration and about any changes to this system through sub-regulatory mechanisms, such as web postings, listserv messages, and webinars.
As part of CMS’ efforts to improve the Hospice Compare website, the agency is finalizing its proposal to post information from other publicly available government data sources, such as CDC and NIH, to the website as soon as FY 2020. This would be in addition to the data from the public use file and other CMS data sources.


