On April 19, 2019, the Centers for Medicare and Medicaid Services (CMS) released the proposed rule for FY 2020 payment and quality program updates for skilled nursing facilities (SNFs). CMS estimates that Medicare payment to SNFs will increase by $887 million in FY 2020. The market basket update is to increase by 2.5 percent. SNFs that fail to meet the reporting requirements will have a 2 percent penalty applied to their SNF payments. As finalized in the FY 2019 SNF final rule, CMS adopted the Patient Driven Payment Model (PDPM) to adjust payments made to SNFs based on the patient’s diagnosis and other services required to manage comorbidities, effective October 1, 2019. Under the current methodology, CMS adjusts payments based on the number of minutes of therapy received. CMS proposes the following unadjusted federal rates based on the PDPM:
| Rate Component | Physical Therapy
case-mix |
Occupational Therapy
case-mix |
Speech-Language Pathology case-mix | Nursing case-mix | Non-Therapy Ancillaries case-mix | Non-Case Mix |
| FY 2020 Unadjusted Per Diem Amount – Urban | $61.16 | $56.93 | $22.83 | $106.64 | $80.45 | $95.48 |
| FY 2020 Unadjusted Per Diem Amount – Rural | $69.72 | $64.03 | $28.76 | $101.88 | $76.86 | $97.25 |
Comments are due on June 18, 2019.
CMS Proposes to Loosen Definition of Group Therapy in SNF Setting
CMS proposes to change the definition of group therapy under the SNF Part A benefit from exactly four patients to between two and six patients performing the same or similar activities. CMS is proposing this change in an attempt to better align therapy across settings while providing greater flexibility to therapists.
CMS Proposes Sub-Regulatory Process to Update ICD-10 Codes used Under PDPM
Under the establishment of PDPM, ICD-10 codes are used to assign patients into case-mix groups instead of by the traditional volume of services. As ICD-10 codes have the opportunity to be updated twice annually, CMS proposes to update nonsubstantive ICD-10 codes via the PDPM website. Further, CMS proposes to use this new sub-regulatory pathway for nonsubstantive changes only, while maintaining the current rulemaking process for substantive changes to the ICD-10 code set.
No Substantial Changes Proposed for SNF Value-Based Purchasing Program
Under the SNF Value-Based Purchasing Program (VBP), Medicare payments are to be reduced by two percent, and 60 percent of these funds are to be reallocated as incentive payments based on SNFs’ performance scores. For FY 2020, CMS estimates that the low-volume adjustment policy will increase this payback percentage by 1.51 percent. The SNF VBP Program is estimated to result in $213.6 million in Medicare savings. CMS did not propose any updates to the SNF VBP scoring policies.
CMS is also proposing to change the name of the SNF VBP Program measure, “Skilled Nursing Facility 30-Day Potentially Preventable Readmissions,” to “Skilled Nursing Facility 30-Day Potentially Preventable Readmission after Hospital Discharge,” to differentiate between the readmissions measures in the SNF VBP and QRP programs.
CMS Proposes Expanding Window for Completion of Initial Patient Assessment
CMS currently requires a functional assessment of patients no later than 5 days after admission to a SNF; CMS has always recognized a 3-day grace period for assessment competition. CMS is proposing to formally expand this assessment requirement from 5 days to 8 days.
Two New Quality Measures Proposed for SNFs, Targets Communication of Health Information in PAC
CMS proposes two new process measures, under the new measure domain “Transfer of Health Information” for inclusion in the SNF QRP for 2022:
- Transfer of Health Information to the Provider–Post-Acute Care (PAC)
- Transfer of Health Information to the Patient–Post-Acute Care (PAC)
CMS proposes to update the Discharge to Community-PAC quality measures to exclude baseline nursing facility residents. CMS is requesting public comment on these new and updates measures.
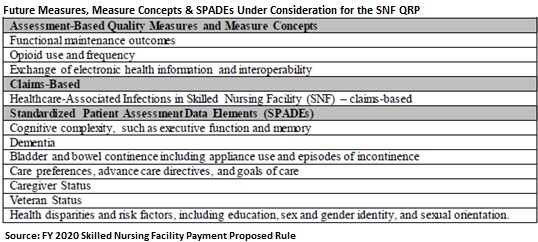
CMS Seeks Input on Standardized Patient Assessment Data Elements (SPADE); Includes Functional Maintenance Outcomes & Pain Interference
CMS is specifically seeking input via an RFI on the SPADEs listed below in Table 13. CMS intends to use this information for policy development in subsequent years. However, CMS proposes that in 2022, PAC providers must report SPADEs.
CMS Asks for Input on Pain Interference
In the ongoing effort to combat the opioid crisis, CMS proposes to standardize pain assessment in post-acute care (PAC) patients. CMS emphasizes the importance of quality pain management through alternative and supplemental therapies for minimizing unnecessary prescription of opioids and finds “pain interference” metric to be more appropriate measurement than pain intensity or pain frequency in PAC settings. The Agency proposes to define pain interference under medical condition and comorbidity data within the standardized patient assessment data with the following elements: pain effect on sleep, pain interference with therapy activities, and pain interference with day-to-day activities. This aligns with the recently released IRF PPS Proposed Rule.
CMS is also soliciting comments from stakeholders on the wage index used to adjust SNF Prospective Payment System (PPS) and on suppressing public reporting on some SNF information.