
This evening, the Centers for Medicare and Medicaid Services released the 2020 Medicare Physician Fee Schedule (PFS) proposed rule. In the proposed rule, CMS is updating several provisions, but making significant changes to E/M and chronic care management services, citing greater flexibility and increased accuracy in codifying services. Additional updates in this year’s PFS includes new requirements for certain telehealth services and coverage for additional opioid treatment services. CMS is also proposing the creation of MIPS Value Pathways (MVPs) beginning with the 2021 performance year/2023 payment year.
Comments on the proposed rule are due September 27, 2019.
Major Changes to Care Management Outlined; Enables More Beneficiaries to Access Services
Recognizing that care management services, which include transition care management (TCM), chronic care management (CCM), and advance care planning (ACP), have a lack of specificity in their coding and payment, CMS proposes to increase payment for TCM services for beneficiaries after discharge from a facility. CMS also proposes a revision to their current restriction of certain HCPCS codes with TCM services. CMS proposes that the following HCPCS codes be allowable with TCM services:
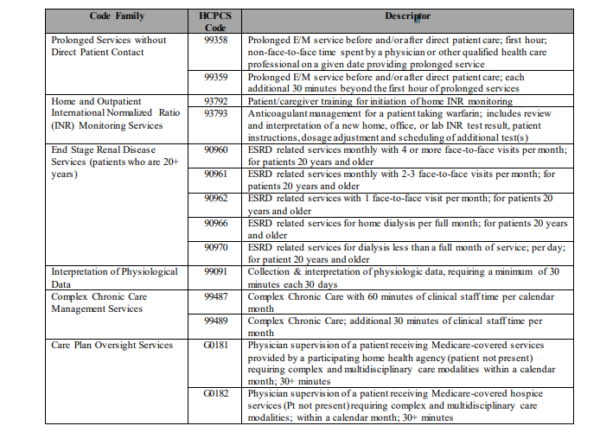
CMS is seeking comment on allowing these HCPCS codes to be billed concurrently with TCM services, specifically whether there is any overlap across the codes.
CMS proposes two new G-codes for Chronic Care Management; seeks feedback pertaining to the transition of these services
CMS proposes two new HCPCS G-codes to describe additional time spent performing chronic care management:
- GCCC1 to reflect the initial 20-minutes of clinical staff time directed by a physician or other qualified health care professional for chronic care management services; and
- GCCC2 to reflect each additional 20 minutes of clinical staff time directed by a physician or other qualified health care professional for chronic care management services
CMS proposes temporary use of these G codes, replacing CPT code 99490, until the CPT Editorial Panel can complete a review a full review of the entire CCM CPT coding set. However, CMS is specifically seeking information on whether these two new temporary codes are too disruptive, and if instead CMS should transition to permanent codes to reflect additional CCM services once AMA’s committee has time to review.
CMS Establishes New Principal Care Management (PCM) Category
Currently, Chronic Care Management (CCM) is only applicable to beneficiaries with more than one complex condition. Recognizing that beneficiaries with only one complex condition can also benefit from CCM services, CMS proposes a new category, PCM, to address ongoing management of beneficiaries with one complex condition. To reflect this new category, CMS proposes two new codes, GPPP1 and GPPP2 to describe chronic care management of PCM.
CMS seeks comments on the creation of this new category, any duplicative payments between proposed PCM services and other care management services, as well as other interprofessional consultation services.
CMS Updates Provisions Pertaining to Evaluation and Management (E/M) Services; Payment Increase Expected
In the 2019 PFS Final Rule, CMS finalized a blended payment rate for E/M CPT codes between levels 2-4, while keeping a separate rate for a level 5 E/M visit. New extended visit E/M add-on codes were also finalized to capture additional time spent with beneficiaries. However, after collecting stakeholder input, CMS proposes to revise their previously-finalized provisions pertaining to E/M codes, and is specifically seeking input on the following proposed provisions:
- Allow clinicians to determine the E/M visit level based on either medical decision-making or time spent with the patient
- Keep 5 levels of E/M services for established patients
- Reduce the number of E/M levels to 4 for office/outpatient E/M visits for new patients
- Revise E/M code definitions to align with the AMA’s CPT Editorial Panel’s recommendations
- Require performance of history and exam only when a clinician determines that it is medically appropriate
- Adopt all of the AMA’s updated RUC recommendations for values of office/outpatient E/M visit codes for CY 2021
- Retain the add-on CPT code for prolonged service time in E/M services, including the ability for this add-on code to be used for primary care and non-procedural specialty services that are part of ongoing management of a patient’s chronic condition(s)
New Face-to-Face requirement for Telehealth Services
CMS proposes to add face-to-face requirements for services described by the following HCPCS codes that currently qualify for telehealth services: GYYY1, GYYY2, and GYYY3. All these HCPCS codes are related to office-based treatment planning and therapy for opioid use disorder. CMS proposes this change as a way to ensure that treatment plans are adequate and relevant to the beneficiary.
CMS Proposes to Cover Methadone and Other Treatment by Opioid Treatment Programs
Currently, a gap in Medicare coverage for methadone treatment for opioid use disorder exists, as methadone may only be administered through an opioid treatment program (OTP). These programs, certified by the Substance Abuse and Mental Health Services Administration (SAMHSA), have not previously been an entity eligible to bill Medicare for services. In its 2019 proposed rule, CMS solicited comments on adding OTPs as eligible Medicare providers, and in this rule, proposes definitions and payment rates for Medicare payment of OTPs.
These providers would be able to dispense methadone, as well as buprenorphine and naltrexone, and provide counseling, therapy, and toxicology testing. Reimbursement would be at a weekly bundled rate determined annually (though CMS solicits comments on daily or monthly bundled payments instead) and based on the costs of the drugs administered plus the services provided. Therapy and counseling would be allowed either in-person or via audio-video equipment. CMS proposes 19 new HCPCS codes to describe these services, with payment ranging from $50.23 for a partial week of non-drug treatment to $5,097 for treatment via buprenorphine implant. The copayment for these services would be $0 for a limited trial period.
CMS Seeks Comment on Bundled Payments, Hints That Updates to Stark Law are Coming
CMS is seeking broad comment from stakeholders on opportunities to expand the concept of bundling payments to increase quality for Medicare beneficiaries, noting desire for better alignment across PFS and other value-based incentive programs.
Last year, CMS issued an RFI on the Stark law, specifically how self-referral limitations can create unnecessary burden and prohibit care-coordination. CMS intends to address these comments related to physician self-referral in separate rulemaking.
CMS Proposes Changes to Scoring Percentage for Two MIPS Category; New MIPS Value Pathway Could be Coming in 2021
In the annual PFS proposed rule, CMS includes its proposals for the Quality Payment Program, which includes two tracks: the Merit-based Incentive Payment Program (MIPS) and Advanced Alternative Payment Models. MIPS includes four performance categories: quality, cost, improvement activities, and promoting interoperability.
For MIPS, CMS is proposing to increase the performance threshold to 45 points for the 2020 performance year, up from 30 points in 2019. The performance threshold is the minimum number of points needed to avoid a negative payment adjustment. CMS is proposing to weight the quality category at 40 percent in 2020 and the cost category at 20 percent; these levels are different from the CY 2019 levels in these categories. The Promoting Interoperability category will remain at 25% and the improvement activities category will remain at 15% for the 2020 performance period.
In addition, CMS is proposing to remove process measures in the quality category and add new episode-based measures in the cost category. Minor changes to the APM track are also being proposed.
CMS Interested in Creating New Pathway for MIPS
CMS is proposing to create the MIPS Value Pathways (MVPs) beginning with the 2021 performance year/2023 payment year. The agency believes that this pathway will decrease clinician burden and improve the quality of performance data. Ultimately, CMS wants to use this framework so that all MIPS eligible clinicians will have to participate through an MVP or a MIPS APM.
An MVP would connect measures and activities across three categories in MIPS: quality, cost, and improvement activities. Initially, a uniform set of Promoting Interoperability measures would be included in all MVPs. These pathways would be organized around specialty or health condition and the quality measures and activities for clinicians would be related to the organization. CMS outlines four guiding principles for the MVPs:
- Consist of a limited set of measures that are important to clinicians, reducing burden related to measure selection, scoring, and leading to sufficient comparative data;
- Include measures that result in comparative performance data that is of value to patients in evaluating clinicians and making care decisions;
- Include measures that encourage performance improvements in priority areas; and
- Reduce barriers to APM participation by using measures that are part of APMs and linking cost and quality measurement.
CMS is requesting stakeholder feedback related to the MVPs, including on MVP construction, measure selection, organization, MVP assignment, and the transition to MVPs.


